Authored by Dr. Leland Jaffe, Associate Dean, and Professor; Published on March 21, 2024
Teaching in the clinical setting is a challenging and rewarding experience that plays a crucial role in shaping the next generation of healthcare professionals. As clinical faculty members, we have the unique opportunity to impart knowledge, serve as role models, foster critical thinking, and inspire a passion for lifelong learning in our students. I’ve worked alongside medical students for the past 10 years in the clinical setting (and 5 years before that in the surgical setting), and I feel that I learn more about being an effective clinical educator each year. These tips are certainly not meant to be comprehensive, just a few strategies that I’ve learned along the way. I hope this post helps foster a discussion among clinical educators about best practices regarding student clinical education in medical school – please comment below with other tips.
To maximize our effectiveness as clinical educators, here are 10 key tips to consider:
1. Establish clear learning objectives:
Before each teaching session in the clinic, take the time to define the learning objectives for your students clearly. These objectives should outline what students are expected to learn and achieve during the clinical course, providing a roadmap for both teaching and assessment. When outlining learning objectives for medical students on their clinical rotations, it’s essential to be clear, specific, and tailored to the individual student’s level of training and clinical experience. Begin by discussing the overarching goals of the rotation and how they align with the student’s educational objectives. Break down the learning objectives into measurable and achievable milestones, focusing on key clinical skills, knowledge areas, and competencies that the student should aim to achieve during the rotation.
Further, encourage active participation and self-reflection by involving the student in the goal-setting process and periodically reviewing progress towards the objectives. Provide opportunities for feedback and guidance throughout the clinical activities to support student learning and growth. By clearly outlining learning objectives and providing guidance and support, educators can empower medical students to make the most of their clinical rotations and achieve their educational goals I attempt to identify where the students are in their medical education and attempt to elevate their knowledge slightly. I say slightly because if you teach at a fellowship level to a 2nd-year student, you’re likely to lose them in your teachings. We should allow students to rely on their previous knowledge and elevate it a few notches.
2. Foster a supportive learning environment:
Create a supportive and inclusive learning environment where students feel comfortable asking questions, seeking clarification, and sharing their perspectives. Encourage open communication, active participation, and mutual respect among students and clinical faculty. Treating medical students with respect in a clinical learning environment is a matter of professional courtesy and crucial for their growth and development as future physicians. Respectful treatment fosters a positive learning environment where students feel valued, supported, and empowered to learn and excel. When students are treated with respect, they are more likely to actively engage in their education, ask questions, seek feedback, and take on greater responsibilities.
Moreover, respectful interactions between faculty members and students serve as role models for professional behavior and communication skills, shaping students’ attitudes and behaviors toward their future patients and colleagues. Ultimately, by treating medical students with respect, clinical educators contribute to the cultivation of a culture of mutual respect, professionalism, and excellence in patient care within the medical community.
Treating medical students disrespectfully during their clinical training can have detrimental effects on their learning and overall well-being. When students experience disrespect from their clinical educators, it can erode their confidence, undermine their motivation to learn, and diminish their sense of belonging within the medical community. Disrespectful behavior may also create a hostile learning environment, inhibiting students’ ability to ask questions, seek clarification, or voice concerns about patient care. Moreover, it can lead to feelings of anxiety, stress, and burnout among students, negatively impacting their mental health and overall academic performance. Ultimately, disrespectful treatment not only hinders students’ learning but also perpetuates a culture of incivility and undermines the principles of professionalism and compassionate patient care within the medical profession.
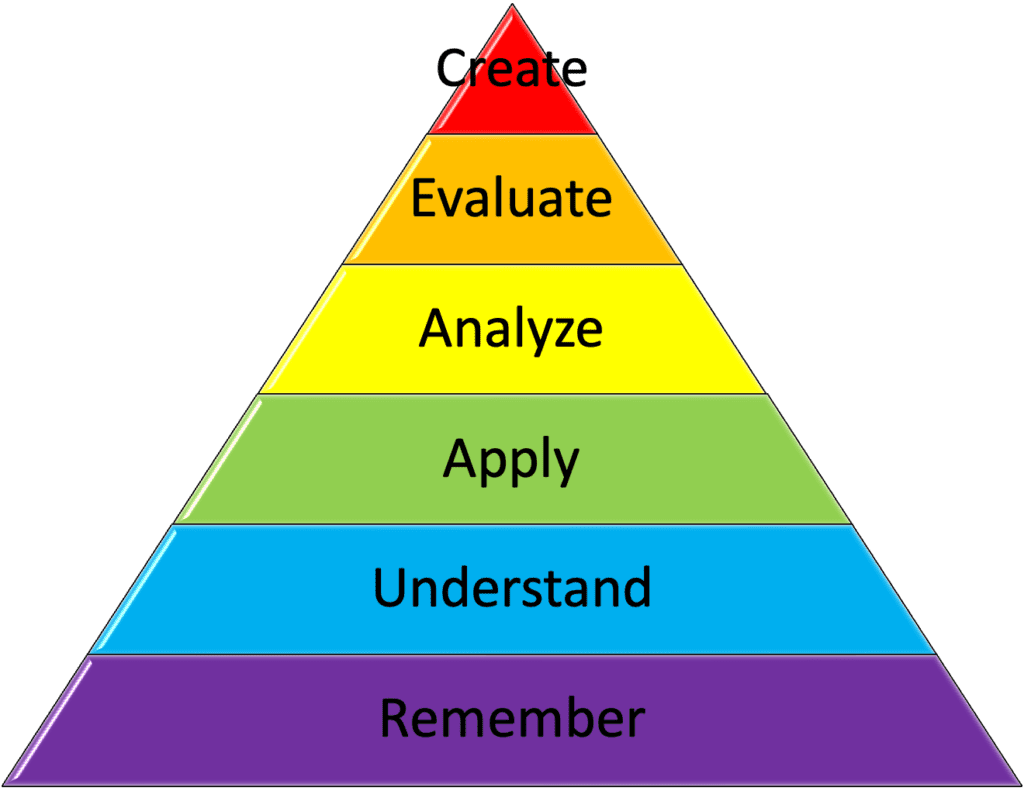
3. Encourage active learning:
Engage students in active learning activities that promote critical thinking, problem-solving, and clinical reasoning skills. Incorporate case studies, role-playing exercises, and hands-on experiences to enhance student engagement and retention of knowledge. Teaching professional students (adult learners) requires a different approach given the practical and real-world applications of their fields. Active learning encourages students to actively participate in their learning process, fostering a deeper understanding of concepts and preparing them for the challenges they will face in their future careers.
Here are a few examples of active learning exercises that can be utilized in the clinical setting:
Case-Based Discussions: Present students with real or simulated patient cases and engage them in group discussions to analyze the clinical presentation, differential diagnosis, and management plan. Encourage students to actively participate by asking probing questions, sharing their insights, and discussing evidence-based approaches to patient care.
Bedside Teaching Rounds: Conduct bedside teaching rounds where students actively participate in patient care activities, such as history-taking, physical examination, and diagnostic reasoning. Encourage students to formulate clinical questions, propose management strategies, and present their findings to the team in a collaborative manner.
Problem-Based Learning (PBL): Implement problem-based learning sessions where students work in small groups to solve clinical problems or cases. Provide students with relevant patient data, diagnostic tests, and treatment options, and challenge them to apply their knowledge to develop a comprehensive management plan and make appropriate clinical decisions.
Simulation-Based Learning: Utilize simulation-based learning activities, such as mannequin simulations or standardized patient encounters, to create immersive and interactive learning experiences in a practice environment. Allow students to practice clinical skills, communication techniques, and teamwork in a controlled environment while receiving feedback from faculty and peers. The use of simulation allows students to practice their clinical skills in a low-pressure environment and helps prepare them for real patients.
Team-Based Learning (TBL): Implement team-based learning sessions where students collaborate in small groups to complete pre-assigned readings, quizzes, or case studies. Facilitate group discussions, encourage peer teaching and learning, and provide immediate feedback on students’ understanding and performance.
Journal Club Discussions: Organize journal club sessions where students critically appraise and discuss recent research articles or clinical guidelines relevant to their specialty. Encourage students to evaluate the strength of evidence, identify potential biases, and discuss the implications of the findings for clinical practice.
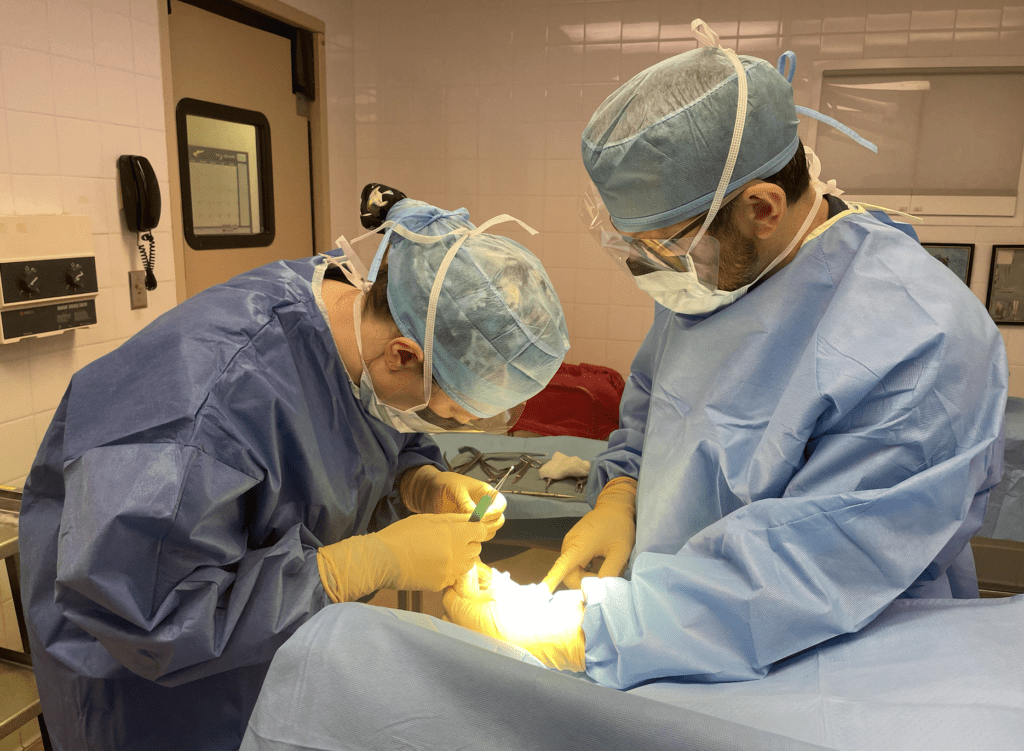
Activities to help develop students’ psychomotor skills such as suture clinic, hand-ties, and physical examination practice, among many other skills.
4. Provide constructive feedback:
In the clinical training setting, feedback plays a crucial role in shaping students’ learning and professional development. Constructive feedback is characterized by its focus on specific behaviors, actionable recommendations for improvement, and a supportive tone that fosters growth and self-reflection. It highlights areas of strength and provides clear guidance on areas for improvement, helping students identify their strengths and weaknesses and develop strategies for growth. In contrast, non-constructive feedback is vague, subjective, and lacks actionable insights, making it less helpful for students’ learning and development. It may focus on personal characteristics rather than observable behaviors, leading to feelings of frustration, demotivation, and confusion among students. By providing constructive feedback that is specific, actionable, and delivered with empathy and respect, educators can empower students to thrive in their clinical training and become competent, compassionate healthcare professionals.
5. Be a role model:
Lead by example and demonstrate professionalism, empathy, and compassion in your interactions with patients, colleagues, and students in the clinical environment. Serve as a positive role model for students, exemplifying the values and behaviors of a competent and compassionate healthcare professional. In my experience, students will notice my interactions and productive positive relationships with my patients and will work to emulate those behaviors.
6. Emphasize patient-centered care:
Emphasize the importance of patient-centered care and the holistic approach to patient management. Encourage students to consider the unique needs, preferences, and values of each patient and involve them in shared decision-making whenever possible. This becomes especially true when discussing the social determinants of health with students and how this can impact the trajectory of a patient’s health.
7. Promote lifelong learning:
Instill a culture of lifelong learning in your students by emphasizing the importance of staying up-to-date with the latest evidence-based practices, guidelines, and advancements in healthcare. Encourage students to seek out opportunities for continuing education and professional development throughout their careers. This circles back to the importance of journal clubs and other activities to discuss and work toward implementing evidence-based medicine. I try to emphasize the importance of staying curious, adaptable, and open to new ideas and perspectives throughout their medical careers. By fostering a culture of lifelong learning in medical education, you can empower students to become lifelong learners who are equipped to meet the ever-evolving challenges of healthcare and make meaningful contributions to the field.
8. Use technology effectively:
Leverage technology to enhance teaching and learning in the clinical setting. Utilize electronic health records, medical simulation tools, virtual patient encounters, and other innovative technologies to provide students with immersive learning experiences and exposure to real-world clinical scenarios.
9. Encourage reflection and self-assessment:
Encourage students to engage in reflection and self-assessment of their clinical skills, knowledge, and attitudes. Provide opportunities for students to critically reflect on their experiences, identify areas for growth, and develop strategies for self-improvement. Self-reflection is a cornerstone of professional education, offering students invaluable opportunities to assess their knowledge, skills, and attitudes, and identify areas for growth and improvement. Through self-reflection, professional students gain insights into their strengths and weaknesses, enhance their self-awareness, and develop a deeper understanding of their professional identity and values. Moreover, self-reflection fosters lifelong learning habits by encouraging students to continuously evaluate their experiences, seek feedback, and adapt their practice to meet evolving challenges and expectations in their respective fields.
10. Collaborate with interdisciplinary teams:
Emphasize the importance of interdisciplinary collaboration and teamwork in healthcare delivery. Provide opportunities for students to collaborate with colleagues from other health professions such as nursing, podiatry, pharmacy, physician assistant, and physical therapy, along with osteopathic and allopathic health, to promote effective communication, coordination of care, and patient safety. I have the privilege of working in an interdisciplinary wound care center where I practice alongside wound ostomy care nurses, an infectious disease doctor, internal medicine doctors, nurse practitioners, interventional radiologists, and nutritionists, among others for the betterment of patient care. An interdisciplinary approach to healthcare offers numerous benefits by leveraging the expertise and perspectives of professionals from diverse fields to provide comprehensive and holistic patient care.
By collaborating across disciplines, healthcare teams can enhance patient outcomes through integrated care plans that address the multifaceted needs of patients. This approach fosters communication, teamwork, and mutual respect among healthcare providers, leading to improved coordination of care and reduced medical errors. Additionally, interdisciplinary collaboration promotes innovation and the exchange of ideas, allowing for the development of novel treatment approaches and the implementation of evidence-based practices. Overall, an interdisciplinary approach to healthcare ensures that patients receive personalized, patient-centered care that considers not only their medical needs but also their social, psychological, and cultural factors.
Simplify Complex Tasks Into More Simple Ones
As a general rule in clinical education, simplifying complex tasks is essential for facilitating student learning and ensuring competency in clinical practice. One effective approach is to break down complex tasks into smaller, manageable steps, allowing students to grasp each component before moving on to the next. Providing clear and concise instructions, along with visual aids or demonstrations, can further enhance understanding and retention of information. Additionally, incorporating repetition and practice opportunities allows students to reinforce their skills and gradually build confidence in performing complex tasks independently. Encouraging active participation and offering constructive feedback throughout the learning process can also help students navigate challenges and overcome obstacles more effectively. By employing these strategies, educators can help students develop the competence and confidence needed to tackle complex tasks with ease and proficiency in clinical practice.
The Challenges of teaching students in the clinical setting
I get it! Teaching students in the clinical setting is difficult, time-consuming, and slows the pace of your clinic – what little time we have to relax during a busy clinical day is taken by teaching responsibilities. One of the primary difficulties is finding dedicated time for teaching amidst the demands of patient care and administrative responsibilities. The busy clinical setting and unpredictable nature of clinical environments can make it challenging to plan structured teaching sessions and provide individualized attention to students.
Additionally, limited resources, such as patient availability, equipment, and space, can further constrain teaching opportunities. Furthermore, balancing the need for students to gain hands-on experience with the imperative to ensure patient safety and privacy adds another layer of complexity to clinical teaching. Despite these challenges, educators must find creative solutions and leverage opportunities for teaching to ensure that students receive high-quality education and mentorship in the clinical setting. What challenges have you faced in attempting to provide high-quality clinical education to your students?
Tips For Teaching Students In The Clinical Setting – Conclusion


By incorporating these tips into your clinical teaching methods, you can create a positive and enriching learning experience for your students, empowering them to become competent, compassionate, and lifelong learners in the field of healthcare. In my experience, effective clinical teaching methods will be different for different types of learners. I will try to incorporate different strategies from this list to get the most out of my students. Together, we can inspire the next generation of healthcare professionals and make a meaningful impact on their patients’ lives.